
Triggered by air, food, and environmental toxins, new diagnoses are being considered as the root cause of chronic disease. – istockphoto
WHAT IS IT?
Multiple chemical sensitivity (MCS), “environmental illness,” “environmental sensitivity,” or “idiopathic environmental intolerance” (IEI), each refer to a variety of symptoms experienced by people after exposure to chemical, biologic, or physical substances.
In 1996 the World Health Organization proposed using the phrase “idiopathic environmental intolerance” (IEI) instead of MCS, because many people attribute symptoms to environmental agents other than chemicals, such as food or electromagnetic forces. MCS or IEI is fairly common in the United States.
 Cigarette smoke, food colorings, alcohol, paint, pesticides, gasoline, plastics, car exhaust fumes, shampoos, caffeine, turpentine, new carpeting, bleach, chemical food additives, household cleaners, fragrances, and newspaper ink are some of the most commonly reported triggers. These common triggers cause severe, debilitating reactions in a MCS/IEI patient whereas the average person might be mildly affected by these products or environmental conditions. Statistical studies show that 16% of people in California and New Mexico report that their IEI or MCS symptoms severely limit their ability to function on a daily basis. Some are unable to leave their homes because of the possibility of having a severe asthmatic reaction to someone wearing perfume in an elevator or at a movie theater, for example. Some cannot live in an apartment complex because of the gas heat, or because of neighbors who smoke cigarettes. Some are never unable to open their windows because of car exhaust or the gas fumes from neighborhood lawn mowers. Some cannot ever eat food prepared in public restaurants or packaged foods due to chemical food additives, resulting severe symptoms such as fainting or vomiting. This can lead to isolation and depression. Many have multiple combinations of environmental sensitivities, dramatically limiting their abilities to function.
Cigarette smoke, food colorings, alcohol, paint, pesticides, gasoline, plastics, car exhaust fumes, shampoos, caffeine, turpentine, new carpeting, bleach, chemical food additives, household cleaners, fragrances, and newspaper ink are some of the most commonly reported triggers. These common triggers cause severe, debilitating reactions in a MCS/IEI patient whereas the average person might be mildly affected by these products or environmental conditions. Statistical studies show that 16% of people in California and New Mexico report that their IEI or MCS symptoms severely limit their ability to function on a daily basis. Some are unable to leave their homes because of the possibility of having a severe asthmatic reaction to someone wearing perfume in an elevator or at a movie theater, for example. Some cannot live in an apartment complex because of the gas heat, or because of neighbors who smoke cigarettes. Some are never unable to open their windows because of car exhaust or the gas fumes from neighborhood lawn mowers. Some cannot ever eat food prepared in public restaurants or packaged foods due to chemical food additives, resulting severe symptoms such as fainting or vomiting. This can lead to isolation and depression. Many have multiple combinations of environmental sensitivities, dramatically limiting their abilities to function.
WHAT ARE THE SYMPTOMS?
The symptoms of MCS/IEI vary from patient to patient but the most common symptoms are respiratory distress, dizziness, gastrointestinal problems, joint pain, fatigue and severe headache.

People who suffer with MCS/IEI often report having several of the following symptoms:
- burning eyes
- wheezing, breathlessness
- extreme fatigue/lethargy
- headache/migraine
- nausea, upset stomach
- vertigo/dizziness
- fainting
- seizures
- memory problems
- runny nose (rhinitis)
- sore throat
- chronic cough
- sinusitis
- inflammation
- skin rashes and or itching skin
- sensitivity to light & noise
- sensitivity and pain with heat or cold
- insomnia or sleeping disorders
- diarrhea or constipation
- bloating
- sweating profusely or uncontrollable chills
- food sensitivities and/or irritable bowel syndrome
- muscle & joint pain
- trouble concentrating, foggy-headed
 WHO IS MOST LIKELY TO EXPERIENCE MCS/IEI?
WHO IS MOST LIKELY TO EXPERIENCE MCS/IEI?
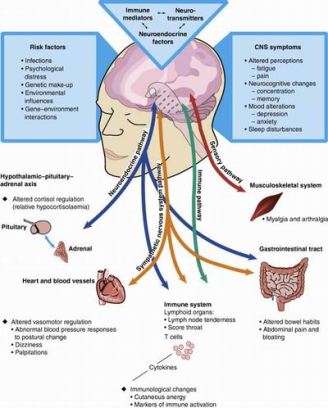
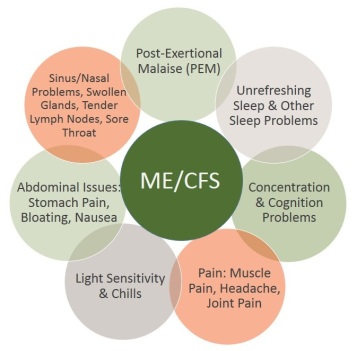
MCS/IEI can affect people of all ages. There appears to be a link between fibromyalgia or chronic fatigue syndrome patients and MCS/IEI patients. MCS/IEI patients and ME/CFS/CFIDS/PVFS (myalgic encephalomyelitis – chronic fatigue) patients have very similar symptoms. Because the symptoms are so similar, it is not easy for doctors to make an accurate diagnosis. When surveying a general population of people with CFS, it was determined that 14% of MCS patients also had CFS and 41% of CFS patients met criteria for MCS diagnosis.
People with a history of allergies, sinusitis, or food intolerances or sensitivities are more likely to experience MCS/IEI. Chronic Fatigue Syndrome (CFS) patients also report worsening of allergies when exposed to chemicals and environmental triggers. This may be related to a CFS/MCS/IEI diagnosis.
Research studies show that Veterans of the Persian Gulf War and people diagnosed with Gulf War illnesses (GWI) report chemical sensitivities at a three-times higher rate than civilians or veterans who did not participate in the Gulf War, or non-deployed veterans. Those who were profoundly affected by hurricane Katrina and other natural disasters, also reported to have MCS/IEI symptoms. There may be a connection between post-traumatic stress disorder and MCS/IEI.
WHAT IS THE CAUSE OF MCS/IEI?
 The cause of MCS/IEI is yet to be determined. Some believe that it is the result of an incident which resulted in toxic exposure from one particular source, and developed into what is known as “spreading.” “Spreading” is a phenomenon where the body becomes sensitive to other chemicals as a result of exposure to one chemical. This phenomenon is characteristic of veterans who have MCS/IEI and also diagnosed with Gulf War illness, or others who have had a traumatic event in their lives.
The cause of MCS/IEI is yet to be determined. Some believe that it is the result of an incident which resulted in toxic exposure from one particular source, and developed into what is known as “spreading.” “Spreading” is a phenomenon where the body becomes sensitive to other chemicals as a result of exposure to one chemical. This phenomenon is characteristic of veterans who have MCS/IEI and also diagnosed with Gulf War illness, or others who have had a traumatic event in their lives.
It is also believed that the MCS/IEI reaction can be a result of long-term exposure to toxic chemicals, such as those who work factories or live in heavily polluted city environments. It is also a possibility that MCS/IEI is a psychological reaction rather than a biochemical reaction although the symptoms can be quite debilitating, often resulting in the person living a completely isolated lifestyle. It is also possible that MCS/IEI is an autoimmune disorder. More research is needed to determine the cause.
Some researchers believe that MCS/IEI is a misdiagnosis for another disorder. More than half of 54 people from one MCS study were mistakenly diagnosed with MCS, and instead were determined to have a somatoform disorder or panic disorder. Migraine, anxiety disorder, lupus, postural orthostatic tachycardia syndrome or other forms of orthostatic intolerance, hay fever and other allergies, hypercalcemia, hypothyroidism, chronic fatigue syndrome, fibromyalgia, or mast cell activation diseases such as mastocytosis, or any disease or condition where symptoms can be triggered by environmental toxins, chemicals or inhalants, could be possible reasons for a MCS/IEI misdiagnosis.
DIAGNOSIS OF MCS/IEI
The definition of MCS /IEI was established by researchers and clinicians in 1999. Specific symptoms are not listed in the criteria, however respiratory symptoms, gastrointestinal symptoms, fatigue, weakness, and headaches are most common. The following six criteria must be present for a person to be diagnosed with MCS/IEI:
- The symptoms are reproducible with repeated exposure to the same chemical.
- The condition is chronic.
- Low levels of exposure (lower than previously or commonly tolerated) result in manifestations of the syndrome.
- The symptoms improve or resolve when the incitants (irritating agent such as a virus, bacterium, prion, gas, or fungus) are removed.
- Responses occur to multiple chemically unrelated substances.
- Symptoms involve multiple organ systems (most commonly the neurological, immune, respiratory, skin, gastrointestinal and musculoskeletal).
 CONTROVERSY ABOUT MCS/IEI
CONTROVERSY ABOUT MCS/IEI
The International Statistical Classification of Diseases and Related Health Problems (ICD), maintained by the World Health Organization, does not recognize MCS or environmental sensitivity as a valid diagnosis. The American Medical Association (AMA) has stated that MCS is not recognized as an established organic disease. The American Academy of Allergy, Asthma, and Immunology, the California Medical Association, the American College of Physicians, and the International Society of Regulatory Toxicology and Pharmacology also do not recognize it as a medical diagnosis or disease.
However, In 1997, U.S. Social Security Administration Commissioner John Callahan issued a court memorandum officially recognizing MCS “as a medically determinable impairment.” The SSA agrees that some MCS patients are too disabled to be meaningfully employed.
IS MCS/IEI ACCEPTED UNDER THE AMERICANS WITH DISABILITIES ACT?
The ADA does not list particular disabilities accepted under the Americans with Disabilities Act, however, some people with MCS/EI will have a disability under the ADA and some will not, depending on the severity of their symptoms. If a person’s MCS/IEI is disabling, then the employer is required by law to make accommodations. For more information about how to determine whether a person has a disability under the ADA, and suggestions as to how to work with your employer to modify your working environment, visit the Job Accommodations Network.

TREATMENT AND LIFESTYLE CHANGES
Lifestyle changes are the primary treatment for most MCS/IEI sufferers. A 2003 survey of 917 MCS patients concluded that the two most effective treatments for MCS were a chemical-free living space and chemical avoidance. Prayer and meditation also were recommended choices. Of those who tried Zoloft, prescription medication, two-thirds of patients reported it as being harmful, along with other pharmaceutical drugs and chemical, unnatural solutions.
Nutritional or dietary changes, including vitamin or herbal supplements, can also be beneficial. Many people with MCS/IEI with dietary restrictions might eliminate whole categories of foods (dairy, for example, or meat). A trusted nutritionist or healthcare practitioner can work with the patient to review and plan a diet with optimal nutrition.
In addition to meditation, dietary and lifestyle changes, some patients suffering from MCS/IEI symptoms have found acupuncture, chiropractic treatment, or yoga to be effective methods for relieving respiratory, anxiety, nausea, and pain symptoms and promoting relaxation.
However, the primary treatment remains to take action to modify the living environment and avoid MCS/IEI triggers. The following modifications may be effective:
- Vacuum pillows, beds, chairs, etc. weekly, with a HEPA filter vacuum, change the filter regularly
- Wash sheets and blankets weekly in hot water (130°F [54°C]) and dry in a hot dryer.
- Cover mattresses and pillowcases with airtight allergen-proof covers.
- Replace comforters and pillows made from natural materials (such as down, feathers, or cotton) with those made from synthetic fibers.
- Avoid wall-to-wall carpeting (especially in the bedroom) as much as possible. If you have it, be sure to vacuum often.
- Throw out all products with chemical fragrances (perfumes, cleaning supplies, shampoo, etc.)
- Buy only natural, fragrance-free products
- Close all open gaps in windows, floorboards, doors, and around drains.
- Fix and seal leaky water faucets and pipes because roaches need water and humidity to survive.
- Always keep food in airtight containers.
- Remove pet food dishes after pets have eaten.
- Keep stove and kitchen surfaces free of food and dirt.
- Use an air-purifier with a HEPA filter
- Throw out all food products with food additive and chemicals
- Do not use processed oils
- Wash all fresh fruits and vegetables before eating
- Do not eat packaged foods.
- Remove any curtains, carpeting, or wallpaper that show visible evidence of mold.
- Install exhaust fans in the kitchen and bathroom.
- Use dehumidifiers in damp areas such as the basement, and hire others to clean this regularly
- Avoid storing clothing in damp areas.
- Do not carpet damp or concrete floors, use wooden floors or tile floors only, if possible
- Do not use gas stoves or gas heating, use electric
- Do not use synthetic, plastic or man-made fibers in clothing or blankets.
- Use a solution of 1 part bleach and 20 parts water to clean areas with mold.
- Do not frequent any locations that allow smoking.
- Avoid areas with fresh paint fumes.
- Avoid the fumes of strong cleaning products.
- Avoid perfumes and aerosols.
- Use masks if needing to go around airport terminals, bus stations or train stations, or hire others to help you.
- Hire others to help you with raking, mowing, blowing leaves, gardening and cleaning the garage, yard or home.
- Close windows and stay indoors (with air conditioning) when necessary, using air purifiers.
- Have an air quality test performed by an industrial hygiene professional to assess poor air quality, dust, mold or mildew accumulation, VOC concentration, etc.
- Buy indoor exercise equipment to keep physically fit rather than participating in outdoor activities
- Make your home a pleasant enjoyable place where you can meet your needs and best care for yourself in comfort.
RESEARCH ARTICLES
Principles and Methods for Assessing Autoimmunity Associated With Exposure to Chemicals: Environmental Health Criteria 236 – ehc236.pdf. World Health Organization (WHO)
Watanabe M, Tonori H and Aizawa Y, “Multiple chemical sensitivities and idiopathic environmental intolerance” (part one), Department of Preventive Medicine and Public Health, Kitasato University School of Medicine, 1-15-1 Kitasato, 228-8555 Sagamihara, Kanagawa, Japan, Environ Health Prev Med, v.7(6); Jan 2003, PMC2723465
Watanabe M, Tonori H and Aizawa Y, “Multiple chemical sensitivities and idiopathic environmental intolerance” (part two), Department of Preventive Medicine and Public Health, Kitasato University School of Medicine, 1-15-1 Kitasato, 228-8555 Sagamihara, Kanagawa, Japan, Environ Health Prev Med, v.7(6); Jan 2003, PMC2723466
Meggs WJ, Dunn KA, Bloch RM, et al. Prevalence and nature of allergy and chemical sensitivity in a general population. Arch Environ Health 1996; 51:275.
Kreutzer R, Neutra RR, Lashuay N. Prevalence of people reporting sensitivities to chemicals in a population-based survey. Am J Epidemiol. 1999;150:1-12.
Multiple chemical sensitivity: a 1999 consensus. Arch Environ Health. 1999;54:147-9.
Fukuda K, Nisenbaum R, Stewart G, et al. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. JAMA. 1998;280:981-8.
Jason LA, Taylor RR, Kennedy CL. Chronic fatigue syndrome, fibromyalgia and multiple chemical sensitivities in a community-based sample of persons with chronic fatigue syndrome-like symptoms. Psychosom Med. 2000;62:655-63.
Bailer J, Witthöft M, Rist F. Psychological predictors of short- and medium term outcome in individuals with idiopathic environmental intolerance (IEI) and individuals with somatoform disorders. J Toxicol Environ Health A 2008; 71:766.
Sparks PJ, Daniell W, Black DW, et al. Multiple chemical sensitivity syndrome: a clinical perspective. I. Case definition, theories of pathogenesis, and research needs. J Occup Med 1994; 36:718.
Levin AS, Byers VS. Environmental illness: a disorder of immune regulation. Occup Med 1987; 2:669.
Black, DW., Temple S, “Overview of idiopathic environmental intolerance (multiple chemical sensitivity)”
_________________________________
 This article is written by Jean Voice Dart, M.S. Special Education from Illinois State University. Jean is a published author and has written hundreds of health articles as well as hosting a local television program, “Making Miracles Happen.” She is a Registered Music Therapist, Sound Therapist, and Master Level Energetic Teacher, and is the Executive Director, founder and Health and Wellness Educator of the Monterey Bay Holistic Alliance. The Monterey Bay Holistic Alliance is a registered 501 (c) 3 nonprofit health and wellness education organization. For more information about the Monterey Bay Holistic Alliance contact us or visit our website at www.montereybayholistic.com.
This article is written by Jean Voice Dart, M.S. Special Education from Illinois State University. Jean is a published author and has written hundreds of health articles as well as hosting a local television program, “Making Miracles Happen.” She is a Registered Music Therapist, Sound Therapist, and Master Level Energetic Teacher, and is the Executive Director, founder and Health and Wellness Educator of the Monterey Bay Holistic Alliance. The Monterey Bay Holistic Alliance is a registered 501 (c) 3 nonprofit health and wellness education organization. For more information about the Monterey Bay Holistic Alliance contact us or visit our website at www.montereybayholistic.com.
Disclaimer:The Monterey Bay Holistic Alliance is a charitable, independent registered nonprofit 501(c)3 organization and does not endorse any particular products or practices. We exist as an educational organization dedicated to providing free access to health education resources, products and services. Claims and statements herein are for informational purposes only and have not been evaluated by the Food and Drug Administration. The statements about organizations, practitioners, methods of treatment, and products listed on this website are not meant to diagnose, treat, cure, or prevent any disease. This information is intended for educational purposes only. The MBHA strongly recommends that you seek out your trusted medical doctor or practitioner for diagnosis and treatment of any existing health condition.


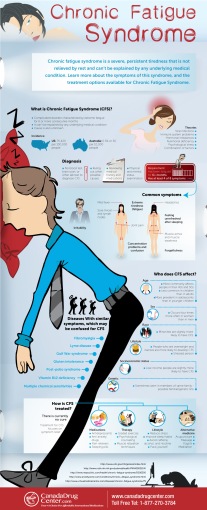


 WHAT IS THE DIFFERENCE BETWEEN CHRONIC FATIGUE SYNDROME AND FIBROMYALGIA?
WHAT IS THE DIFFERENCE BETWEEN CHRONIC FATIGUE SYNDROME AND FIBROMYALGIA?
