DEFINITION OF CHRONIC FATIGUE SYNDROME
DEFINITION OF CHRONIC FATIGUE SYNDROME
Chronic Fatigue Syndrome (CFS) is a complicated disorder characterized by extreme fatigue that is not explained through diagnostic testing or a pre-existing medical condition. CFS is also known as Myalgic Encephalomyelitis (ME), chronic fatigue and immune dysfunction syndrome (CFIDS) and by other names. It can be a complex and debilitating chronic illness with a serious impact on one’s quality of life. Fatigue specific to CFS may worsen with physical or mental activity, but doesn’t improve after sleeping or resting.
WHAT ARE THE SYMPTOMS OF CFS? The most common symptoms of Chronic Fatigue Syndrome or Myalgic Encephalomyelitis (ME/CFS) include post-exertional malaise (PEM). PEM is characterized by a state of exhaustion due to sleep that is not relieved by bedrest or sleep. This unrefreshing sleep leads to trouble concentrating or mental fatigue, joint and muscle pain, with worsening symptoms typically lasting for six months or more.
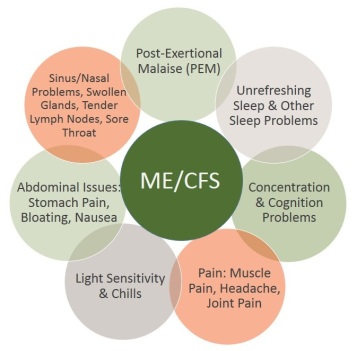 Primary symptoms include:
Primary symptoms include:
- Increased malaise (extreme exhaustion and sickness) following physical activity or mental exertion
- Problems with sleep
- Difficulties with memory and concentration
- Persistent muscle pain
- Joint pain (without redness or swelling)
- Headache
- Tender lymph nodes in the neck or armpit
- Sore throat
Other secondary symptoms may include:
- Brain fog or trouble concentrating
- Difficulty maintaining an upright position
- Dizziness, balance problems or fainting
- Allergies or sensitivities to foods, odors, chemicals, medications, or noise
- Irritable bowel syndrome
- Low grade fever or low body temperature
- Numbness, tingling, or burning sensations in the face, hands, or feet
- Chills and night sweats
- Visual disturbances (sensitivity to light, blurring, eye pain)
- Depression or mood problems (irritability, mood swings, anxiety, panic attacks)
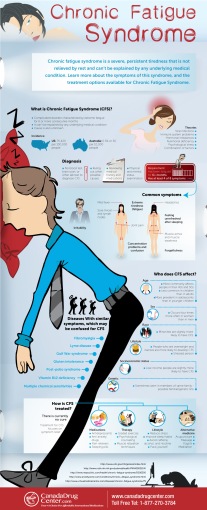 A person with CFS feels completely exhausted to the point of being unable to function. This extreme tiredness makes it hard to do the daily tasks that most of us do without thinking — like dressing, bathing, holding a book, putting away dishes, or eating, and therefore might experience depression. Sleep or rest does not make the tiredness go away. It can be made worse by walking, light exercising, carrying on a conversation or even thinking or problem-solving. Chronic Fatigue Syndrome can happen gradually and worsen over time, or it may occur unexpectedly and suddenly. The extreme tiredness may come and go, over many years. In some cases the CFS symptoms never goes away. CFS symptoms must remain for at least six months before a diagnosis can be made by a trusted physician.
A person with CFS feels completely exhausted to the point of being unable to function. This extreme tiredness makes it hard to do the daily tasks that most of us do without thinking — like dressing, bathing, holding a book, putting away dishes, or eating, and therefore might experience depression. Sleep or rest does not make the tiredness go away. It can be made worse by walking, light exercising, carrying on a conversation or even thinking or problem-solving. Chronic Fatigue Syndrome can happen gradually and worsen over time, or it may occur unexpectedly and suddenly. The extreme tiredness may come and go, over many years. In some cases the CFS symptoms never goes away. CFS symptoms must remain for at least six months before a diagnosis can be made by a trusted physician.
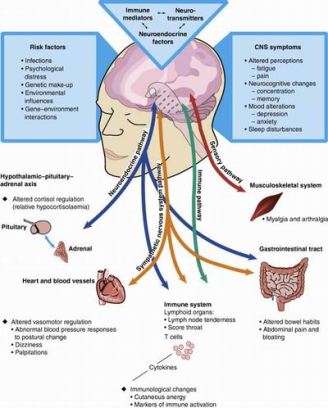
HOW COMMON IS CFS AND WHAT CAUSES IT? Experts estimate that at least one million Americans have CFS, and of these cases, 20% are undiagnosed. Statistics show that in the United States, approximately 75-420 people have CFS per 100,000 people. In Australia, o.3% or 30 per 1,000 people have CFS. Women are four times as likely as men to develop Chronic Fatigue Syndrome and people age 40 – 59 are more likely to be diagnosed, than children. People of all ages can get CFS, although studies suggest that CFS occurs more often in adolescents than in children under twelve years of age. CFS occurs in all ethnic groups, cultures, and countries around the world. Statistics show that it is more  common in lower-income than in higher-income persons, however this is not significant. CFS is sometimes seen in members of the same family. Researchers are determining whether this might be because of a genetic link. People who are overweight and inactive are more likely to develop CFS. There is no definite cause of CFS. Epstein-Barr virus or human herpes virus-6 (HHV-6) might be a contributing factor, however, no specific virus has been identified as the cause. It is thought that it might be caused by inflammation in the nervous system and a faulty immune system response. Age, previous illnesses, stress, genetics, and environmental factors listed above, may also play a significant role in the development of Chronic Fatigue Syndrome. People with Chronic Fatigue Syndrome often report that the onset of symptoms occurred after a time of great stress, such as the loss of a loved one or major surgery. More research is needed to determine the cause.
common in lower-income than in higher-income persons, however this is not significant. CFS is sometimes seen in members of the same family. Researchers are determining whether this might be because of a genetic link. People who are overweight and inactive are more likely to develop CFS. There is no definite cause of CFS. Epstein-Barr virus or human herpes virus-6 (HHV-6) might be a contributing factor, however, no specific virus has been identified as the cause. It is thought that it might be caused by inflammation in the nervous system and a faulty immune system response. Age, previous illnesses, stress, genetics, and environmental factors listed above, may also play a significant role in the development of Chronic Fatigue Syndrome. People with Chronic Fatigue Syndrome often report that the onset of symptoms occurred after a time of great stress, such as the loss of a loved one or major surgery. More research is needed to determine the cause.
 HOW DOES THE DOCTOR DIAGNOSE CFS? A diagnosis of CFS may take many years to determine and can be frustrating or wearing for those suffering from CFS. Laboratory tests currently are not used. Sometimes CFS can be misdiagnosed because many Chronic Fatigue Syndrome symptoms can be side effects of medical treatments or can also be symptoms of other illnesses. Therefore, doctors will prescribe blood and urine tests, and possibly brain MRIs to rule out other illnesses and medical conditions. All adult cases of CFS are determined by the “Fukuda criteria” from the 1994 Centers for Disease Control and Prevention (CDC) definition. Children with CFS are determined by a pediatric case definition of CFS. A qualified doctor will make a diagnosis of CFS after questioning a patient about their physical and mental health, conducting a physical exam, and ordering urine and blood tests to rule-out other medical conditions. The doctor will diagnose a patient as having CFS, only if that person has been extremely tired for six months or more and laboratory test results do not offer a medical solution, and if the patient has four out of the 8 primary symptoms of CFS listed above. In addition to having four out of the eight primary symptoms determined by the Centers for Disease Control and Prevention (listed above under “Primary symptoms”), the patient must also have unexplained, persistent or relapsing chronic fatigue that is:
HOW DOES THE DOCTOR DIAGNOSE CFS? A diagnosis of CFS may take many years to determine and can be frustrating or wearing for those suffering from CFS. Laboratory tests currently are not used. Sometimes CFS can be misdiagnosed because many Chronic Fatigue Syndrome symptoms can be side effects of medical treatments or can also be symptoms of other illnesses. Therefore, doctors will prescribe blood and urine tests, and possibly brain MRIs to rule out other illnesses and medical conditions. All adult cases of CFS are determined by the “Fukuda criteria” from the 1994 Centers for Disease Control and Prevention (CDC) definition. Children with CFS are determined by a pediatric case definition of CFS. A qualified doctor will make a diagnosis of CFS after questioning a patient about their physical and mental health, conducting a physical exam, and ordering urine and blood tests to rule-out other medical conditions. The doctor will diagnose a patient as having CFS, only if that person has been extremely tired for six months or more and laboratory test results do not offer a medical solution, and if the patient has four out of the 8 primary symptoms of CFS listed above. In addition to having four out of the eight primary symptoms determined by the Centers for Disease Control and Prevention (listed above under “Primary symptoms”), the patient must also have unexplained, persistent or relapsing chronic fatigue that is:
- New or definite onset (has not been lifelong)
- Not the result of ongoing exertion
- Not substantially alleviated by rest
- Results in substantial reduction in previous levels of occupational, educational, social, or personal activities.
DISEASES WHICH HAVE SIMILAR SYMPTOMS TO CFS
Doctors must rule out other diseases and chronic illnesses that have similar symptoms. The following diseases and syndromes are often mistaken for Chronic Fatigue Syndrome:
- Drug dependence
- Infections
- Muscle or nerve diseases (such as multiple sclerosis)
- Endocrine diseases (such as hypothyroidism)
- Psychiatric or psychological illnesses, particularly depression
- Tumors
- Fibromyalgia
- Lyme disease
- Gulf War syndrome
- Gluten intolerance
- Post-polio syndrome
- Vitamin B12 deficiency
- Multiple chemical sensitivities
- Other immune or autoimmune disorders
- Heart, kidney or liver diseases
 WHAT IS THE DIFFERENCE BETWEEN CHRONIC FATIGUE SYNDROME AND FIBROMYALGIA?
WHAT IS THE DIFFERENCE BETWEEN CHRONIC FATIGUE SYNDROME AND FIBROMYALGIA?
Chronic fatigue syndrome (ME/CFS) and fibromyalgia (FMS)are alike in many ways. In fact, it is not uncommon for a person to have both fibromyalgia and CFS. Some experts believe that fibromyalgia and CFS are in fact the same disorder. According to the Arthritis Foundation, research shows that 50 to 70 percent of people have both disorders. When diagnosing CFS or fibromyalgia, one primary difference, is determining which symptom is worst – pain or fatigue. The diagnosis could also be influenced by whether your primary care physician or practitioner is more familiar with the American College of Rheumatology’s criteria for FMS or the CDC’s guidelines for ME/CFS. Some researchers have discovered a few significant differences. ME/CFS seems to begin after a person experiences flu-like symptoms, so some believe that chronic fatigued syndrome may be linked to a virus, and those with CFS often have chronic immune system challenges, as if their bodies are fighting an infection, while fibromyalgia patients do not always have this. CFS patients sometimes have low-grade fever and sore throat, while FMS criteria does not require this for a diagnosis. Fibromyalgia is frequently is rooted in a physical or emotional trauma and the pain of FMS often gets better with massage and heat, while the pain of ME/CFS may not necessarily respond favorably to these treatments. However, despite these few differences, many agree that the two diagnoses have multiple similar symptoms and might indeed be the same disorder.
TREATMENT OF CHRONIC FATIGUE SYNDROME
The National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC) are funding CFS research studies on Chronic Fatigue Syndrome in order to determine treatments and cures. The following treatments have been found to be effective Over-the-counter pain relievers such as Aleve, Advil, or Motrin, can be beneficial in reducing pain, such as body aches, headaches, and muscle and joint pain. Non-drowsy antihistamines can help with allergy symptoms, such as sneezing, runny nose, sore throat, nose and watering or itching eyes. Prescription medications like doxepin or amitriptyline can help improve sleep.  Complementary or alternative treatments, such as massage, acupuncture, chiropractic care, yoga, stretching, meditation, Tai Chi, Reiki, biofeedback, or self-hypnosis can be helpful in treating stress-related symptoms or pain. Many alternative treatments, dietary supplements, and herbal remedies can be effective in alleviating CFS symptoms. Neti Pots are a nonprescription solution for chronic allergy and sinusitis problems and recommended for use by most all healthcare practitioners. Herbal remedies such as honey and lemon tea, steam tent, valerian root, grapefruit seed extract, ginger, echinacea, vitamin C supplements, and others. Talk to your doctor, nutritionist, or trusted health-care practitioner in order to determine which treatment is best for you.
Complementary or alternative treatments, such as massage, acupuncture, chiropractic care, yoga, stretching, meditation, Tai Chi, Reiki, biofeedback, or self-hypnosis can be helpful in treating stress-related symptoms or pain. Many alternative treatments, dietary supplements, and herbal remedies can be effective in alleviating CFS symptoms. Neti Pots are a nonprescription solution for chronic allergy and sinusitis problems and recommended for use by most all healthcare practitioners. Herbal remedies such as honey and lemon tea, steam tent, valerian root, grapefruit seed extract, ginger, echinacea, vitamin C supplements, and others. Talk to your doctor, nutritionist, or trusted health-care practitioner in order to determine which treatment is best for you.
Lifestyle changes can be effective in treating CFS. A nutritionist or primary care doctor can make suggestions regarding a healthy diet. A journal can be a helpful tool. Write down what you do each day, noting times when you feel particularly tired. Then, determine which activities are most fatiguing to you. Stop doing things that seem to trigger your tiredness, or do less. If basic tasks are overwhelming, such as dressing or eating, find ways to modify these tasks or break them into smaller steps. 
An occupational therapist or physical therapist can be helpful in recommending assistive devices (such as modified appliances or tools) if you are unable to achieve basic daily life skills. The occupational therapist can help you with setting goals, and choosing alternative approaches to completing tasks at home and at work and making progress in managing your pain and fatigue. You might also need to change your working or resting environment and even move to another location that is more supportive and comfortable for you. CFS affects mental, emotional, or physical energy, so these modifications in behaviors must include all areas of fatigue.
ORGANIZATIONS
- Chronic Fatigue and Immune Dysfunction Syndrome Association of America, Phone: 704-365-2343 http://solvecfs.org/
- Chronic Fatigue Syndrome, Center for Disease Control, Chronic Fatigue Syndrome Advisory Committee, HHS, Phone: 202-690-7650 http://www.cdc.gov/cfs/
- International Association for CFS/ME Phone: 847-258-7248 http://www.iacfsme.org/
- National CFIDS Foundation, Phone: 781-449-3535 http://www.ncf-net.org/
- National Chronic Fatigue Syndrome and Fibromyalgia Association, Phone: 816-737-1343
- The Trans-NIH Working Group on Chronic Fatigue Syndrome, Phone: 301-402-1770
REFERENCES
- Evangard B, Schacterie R.S., Komaroff A. L. (Nov 1999). “Chronic fatigue syndrome: new insights and old ignorance”. Journal of Internal Medicine 246 (5): 455–469.
- Santhouse A, Hotopf M, David AS. Chronic fatigue syndrome. BMJ. 2010;340:c738
- Guideline 53: Chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy). London: National Institute for Health and Clinical Excellence. 2007.
- Afari N, Buchwald D (2003). “Chronic fatigue syndrome: a review”. Am J Psychiatr 160 (2): 221–36
- “Chronic Fatigue Syndrome (CFS), Symptoms”. Centers for Disease Control and Prevention. 2012-05-14. Retrieved 2012-09-23
- “Chronic Fatigue Syndrome Basic Facts”. Centers for Disease Control and Prevention. May 9, 2006. Retrieved 2008-02-07
- Carruthers BM, Jain AK, De Meirleir KL, Peterson DL, Klimas NG, et al. (2003). “Myalgic encephalomyalitis/chronic fatigue syndrome: Clinical working definition, diagnostic and treatment protocols” (PDF). Journal of Chronic Fatigue Syndrome 11 (1): 7–97
- Edmonds M, McGuire H, Price J (2004). “Exercise therapy for chronic fatigue syndrome”. In Price, Jonathan R. Cochrane Database Syst Rev (3): CD003200.
_________________________________
 This article is written by Jean Voice Dart, M.S. Special Education from Illinois State University. Jean is a published author and has written hundreds of health articles as well as hosting a local television program, “Making Miracles Happen.” She is a Registered Music Therapist, Sound Therapist, and Master Level Energetic Teacher, and is the Executive Director, founder and Health and Wellness Educator of the Monterey Bay Holistic Alliance. The Monterey Bay Holistic Alliance is a registered 501 (c) 3 nonprofit health and wellness education organization. For more information about the Monterey Bay Holistic Alliance contact us or visit our website at www.montereybayholistic.com.
This article is written by Jean Voice Dart, M.S. Special Education from Illinois State University. Jean is a published author and has written hundreds of health articles as well as hosting a local television program, “Making Miracles Happen.” She is a Registered Music Therapist, Sound Therapist, and Master Level Energetic Teacher, and is the Executive Director, founder and Health and Wellness Educator of the Monterey Bay Holistic Alliance. The Monterey Bay Holistic Alliance is a registered 501 (c) 3 nonprofit health and wellness education organization. For more information about the Monterey Bay Holistic Alliance contact us or visit our website at www.montereybayholistic.com.
Disclaimer:The Monterey Bay Holistic Alliance is a charitable, independent registered nonprofit 501(c)3 organization and does not endorse any particular products or practices. We exist as an educational organization dedicated to providing free access to health education resources, products and services. Claims and statements herein are for informational purposes only and have not been evaluated by the Food and Drug Administration. The statements about organizations, practitioners, methods of treatment, and products listed on this website are not meant to diagnose, treat, cure, or prevent any disease. This information is intended for educational purposes only. The MBHA strongly recommends that you seek out your trusted medical doctor or practitioner for diagnosis and treatment of any existing health condition.